Evicore Appeal Form
Evicore Appeal Form - Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. Please ensure you are navigating to our most. • providers may provide additional information and request reconsideration from evicore. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. For example, use the prior authorization general request form below if you would like to request a coverage determination (such as a step therapy. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. The request submission form should be used for denied cases. For evicore by evernorth® appeals, review your appeal denial letter for instructions.
• providers may provide additional information and request reconsideration from evicore. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. The request submission form should be used for denied cases. For example, use the prior authorization general request form below if you would like to request a coverage determination (such as a step therapy. Please ensure you are navigating to our most. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. For evicore by evernorth® appeals, review your appeal denial letter for instructions.
The request submission form should be used for denied cases. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. For example, use the prior authorization general request form below if you would like to request a coverage determination (such as a step therapy. For evicore by evernorth® appeals, review your appeal denial letter for instructions. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. • providers may provide additional information and request reconsideration from evicore. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. Please ensure you are navigating to our most.
Fill Free fillable eviCore PDF forms
• providers may provide additional information and request reconsideration from evicore. For evicore by evernorth® appeals, review your appeal denial letter for instructions. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. Formal appeal the.
Fill Free fillable eviCore PDF forms
Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. • providers may provide additional information and request reconsideration from evicore. For evicore by evernorth® appeals, review your appeal.
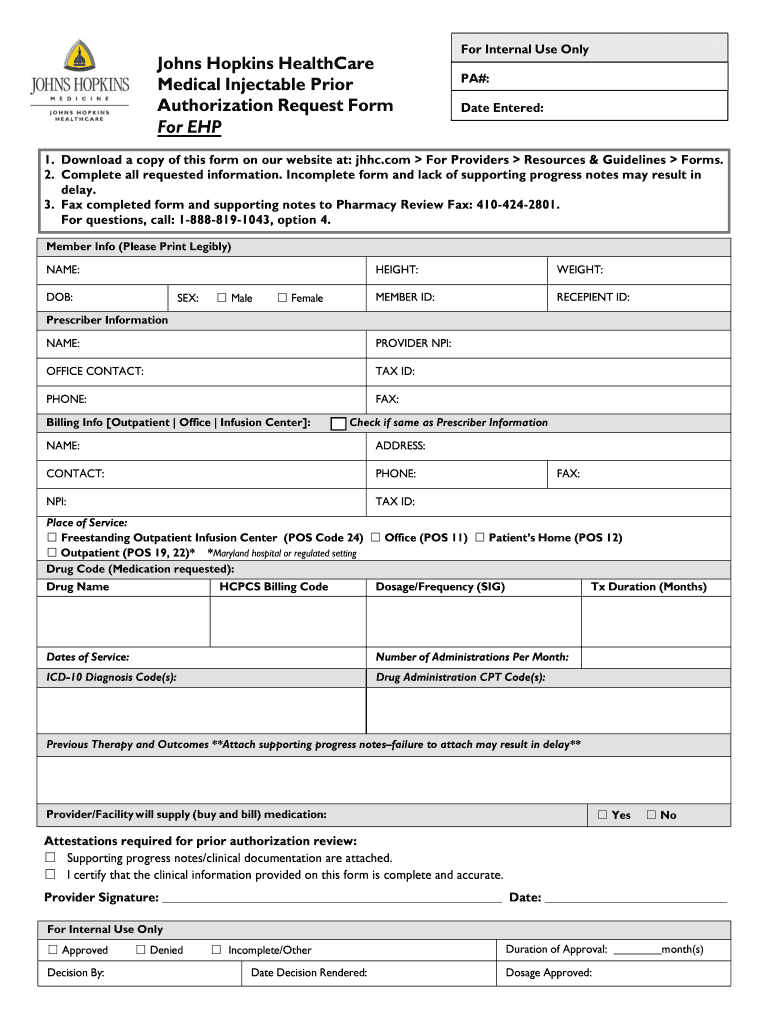
Johns Hopkins Authorization Request Form Fill Online, Printable
For evicore by evernorth® appeals, review your appeal denial letter for instructions. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. The request submission form should be used for denied cases. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from.
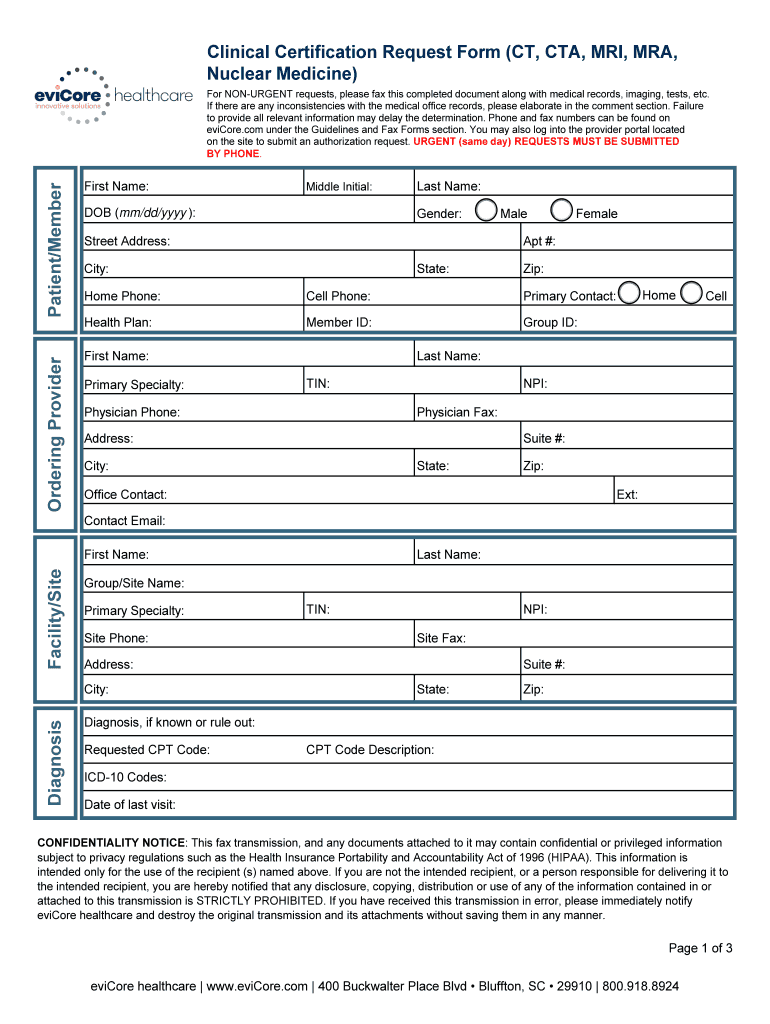
Evicore Certification Request Form Fill Online, Printable, Fillable
Please ensure you are navigating to our most. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. For evicore by evernorth® appeals, review your.
Fill Free fillable eviCore PDF forms
Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. For example, use the prior authorization general request form below if you would like to request a coverage determination (such as a step therapy. • providers may provide additional information and request reconsideration from evicore. Evicore.com recently.
Cigna reconsideration form Fill out & sign online DocHub
Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. Please ensure you are navigating to our most. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the.
Fillable Online Evicore cigna prior authorization form Fax Email Print
The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. The request submission form should be used for denied cases. Please ensure you are navigating to our most. Formal.
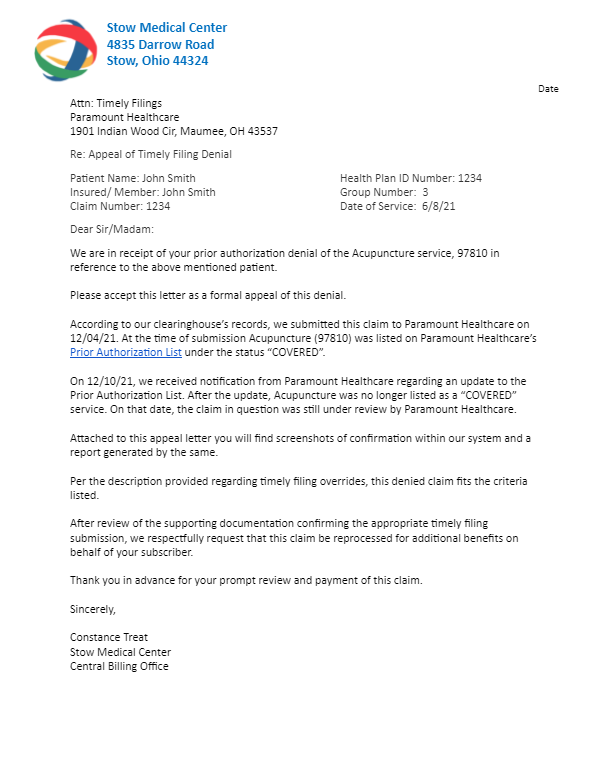
46+ Unitedhealthcare Appeal Letter Sample TanayaMeryl
For evicore by evernorth® appeals, review your appeal denial letter for instructions. Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. The request submission form should be used for denied cases. The required information is outlined on the.
Understanding EviCore's Approach to PatientCentered Care eviCore
The request submission form should be used for denied cases. For evicore by evernorth® appeals, review your appeal denial letter for instructions. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. The required information is outlined on the evicore prior authorization request form and can be.
EviCore Healthcare Lymphedema Program PT/OT Therapy Intake Form 2020
Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan. The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. • providers may provide additional information and request reconsideration from evicore. Please ensure you are.
The Request Submission Form Should Be Used For Denied Cases.
Evicore.com recently upgraded and some of your bookmarked worksheets might have changed. Appeal requests for priority partners members must be submitted to evicore within 60 calendar days from the initial determination. • providers may provide additional information and request reconsideration from evicore. Formal appeal the letter you receive will also outline how you can formally appeal the decision through a process with your health plan.
For Example, Use The Prior Authorization General Request Form Below If You Would Like To Request A Coverage Determination (Such As A Step Therapy.
The required information is outlined on the evicore prior authorization request form and can be accessed on the provider resource page by. For evicore by evernorth® appeals, review your appeal denial letter for instructions. Please ensure you are navigating to our most.





.png)
