Iowa Total Care Prior Authorization Form
Iowa Total Care Prior Authorization Form - Member must be eligible at the time services are rendered. You must fill out the top portion of the outpatient or inpatient. Iowa total care uses prior authorizations to ensure that all care delivered to our members is medically necessary and appropriate, based on. Member must be eligible at the time services are rendered. Anything with an * is required in order for your prior authorization to be submitted. Services must be a covered health plan beneit and medically necessary with prior. Services must be a covered health plan benefit and medically necessary with prior. An authorization is not a guarantee of payment. Services must be a covered health plan benefit and medically necessary with prior authorization as per plan policy and procedures. Find out how to obtain prior authorization for certain services from iowa total care, a medicaid managed care organization.
Find out how to obtain prior authorization for certain services from iowa total care, a medicaid managed care organization. Services must be a covered health plan benefit and medically necessary with prior. Member must be eligible at the time services are rendered. An authorization is not a guarantee of payment. Member must be eligible at the time services are rendered. Member must be eligible at the time services are rendered. Iowa total care uses prior authorizations to ensure that all care delivered to our members is medically necessary and appropriate, based on. Services must be a covered health plan beneit and medically necessary with prior. Services must be a covered health plan benefit and medically necessary with prior authorization as per plan policy and procedures. You must fill out the top portion of the outpatient or inpatient.
Anything with an * is required in order for your prior authorization to be submitted. Services must be a covered health plan benefit and medically necessary with prior. Member must be eligible at the time services are rendered. Member must be eligible at the time services are rendered. Iowa total care uses prior authorizations to ensure that all care delivered to our members is medically necessary and appropriate, based on. You must fill out the top portion of the outpatient or inpatient. An authorization is not a guarantee of payment. Services must be a covered health plan beneit and medically necessary with prior. Services must be a covered health plan benefit and medically necessary with prior authorization as per plan policy and procedures. Find out how to obtain prior authorization for certain services from iowa total care, a medicaid managed care organization.
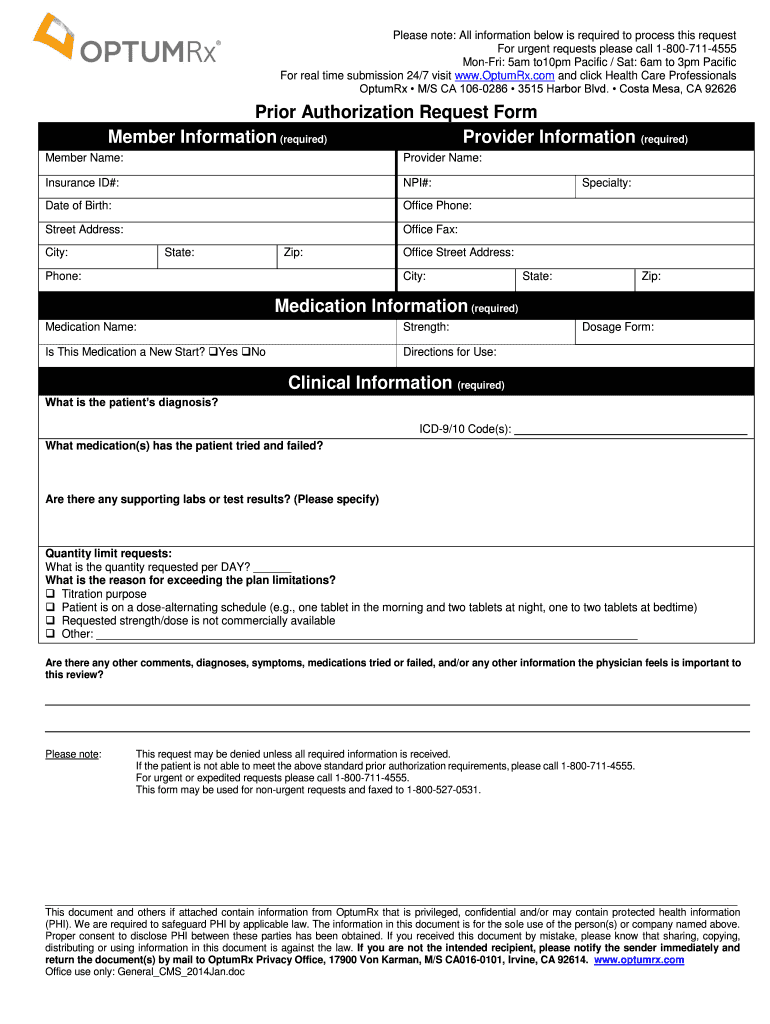
Fillable Online United healthcare prior authorization form pdf Fax
Member must be eligible at the time services are rendered. Services must be a covered health plan benefit and medically necessary with prior. Services must be a covered health plan beneit and medically necessary with prior. Member must be eligible at the time services are rendered. Find out how to obtain prior authorization for certain services from iowa total care,.
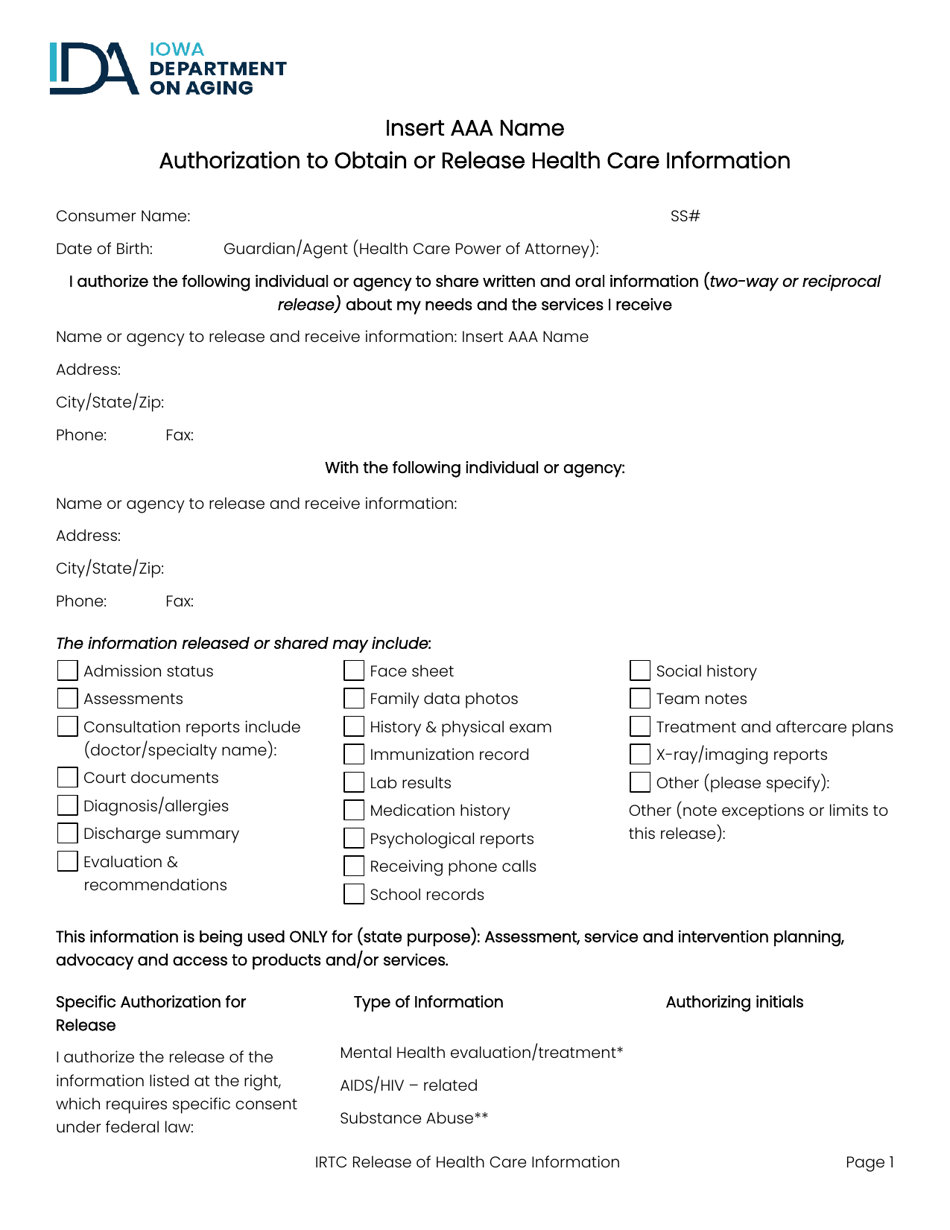
Iowa Authorization to Obtain or Release Health Care Information Fill
Iowa total care uses prior authorizations to ensure that all care delivered to our members is medically necessary and appropriate, based on. Services must be a covered health plan benefit and medically necessary with prior. Member must be eligible at the time services are rendered. An authorization is not a guarantee of payment. You must fill out the top portion.
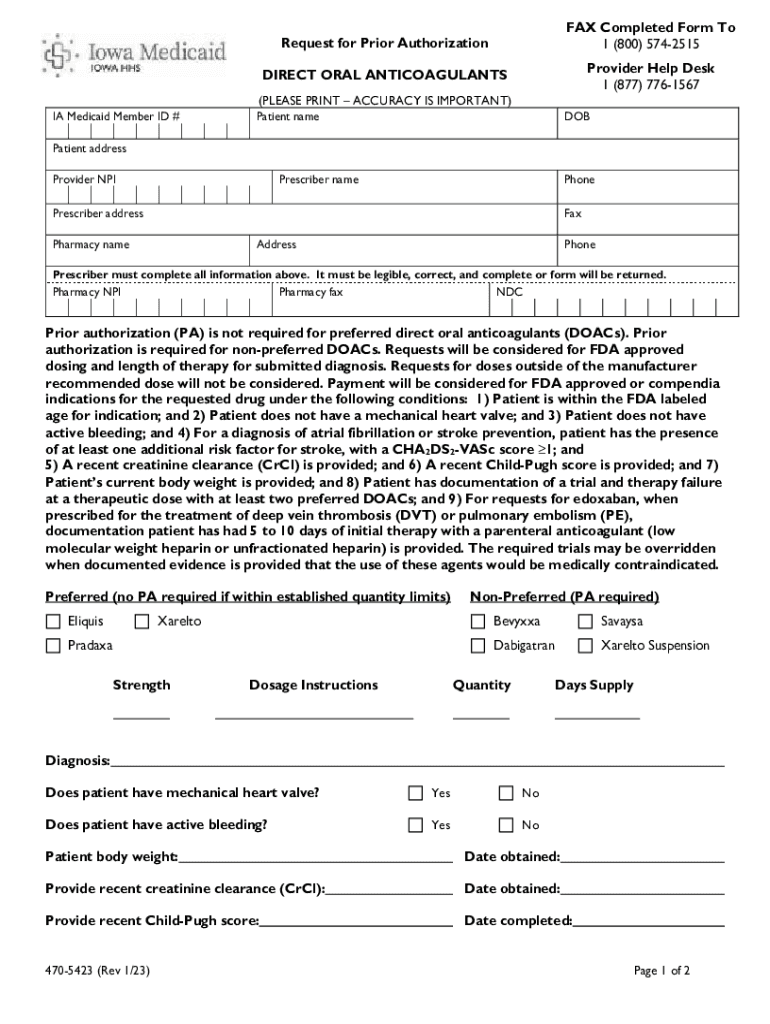
Fillable Online Iowa Medicaid Prior (Rx) Authorization Form eForms
You must fill out the top portion of the outpatient or inpatient. Member must be eligible at the time services are rendered. Services must be a covered health plan benefit and medically necessary with prior authorization as per plan policy and procedures. Anything with an * is required in order for your prior authorization to be submitted. Services must be.
Molina Healthcare Prior Authorization Service Request Form
Services must be a covered health plan beneit and medically necessary with prior. Services must be a covered health plan benefit and medically necessary with prior authorization as per plan policy and procedures. Iowa total care uses prior authorizations to ensure that all care delivered to our members is medically necessary and appropriate, based on. Anything with an * is.
Free Iowa Medicaid Prior (Rx) Authorization Form PDF eForms
Find out how to obtain prior authorization for certain services from iowa total care, a medicaid managed care organization. Iowa total care uses prior authorizations to ensure that all care delivered to our members is medically necessary and appropriate, based on. Member must be eligible at the time services are rendered. Member must be eligible at the time services are.
Medication Prior Authorization Request Form UnitedHealthcare Fill Out
Find out how to obtain prior authorization for certain services from iowa total care, a medicaid managed care organization. Member must be eligible at the time services are rendered. Services must be a covered health plan benefit and medically necessary with prior. Iowa total care uses prior authorizations to ensure that all care delivered to our members is medically necessary.
Blue Shield Promise Health Plan Prior Authorization Form
Find out how to obtain prior authorization for certain services from iowa total care, a medicaid managed care organization. Services must be a covered health plan benefit and medically necessary with prior. Anything with an * is required in order for your prior authorization to be submitted. Member must be eligible at the time services are rendered. Member must be.
Fill Free fillable Absolute Total Care PDF forms
Anything with an * is required in order for your prior authorization to be submitted. Member must be eligible at the time services are rendered. Services must be a covered health plan benefit and medically necessary with prior authorization as per plan policy and procedures. Member must be eligible at the time services are rendered. Member must be eligible at.
Fill Free fillable Absolute Total Care PDF forms
An authorization is not a guarantee of payment. Member must be eligible at the time services are rendered. Services must be a covered health plan beneit and medically necessary with prior. Services must be a covered health plan benefit and medically necessary with prior. You must fill out the top portion of the outpatient or inpatient.
Iowa total care authorization form Fill out & sign online DocHub
Anything with an * is required in order for your prior authorization to be submitted. Find out how to obtain prior authorization for certain services from iowa total care, a medicaid managed care organization. An authorization is not a guarantee of payment. Member must be eligible at the time services are rendered. Iowa total care uses prior authorizations to ensure.
Services Must Be A Covered Health Plan Beneit And Medically Necessary With Prior.
Member must be eligible at the time services are rendered. Iowa total care uses prior authorizations to ensure that all care delivered to our members is medically necessary and appropriate, based on. You must fill out the top portion of the outpatient or inpatient. An authorization is not a guarantee of payment.
Member Must Be Eligible At The Time Services Are Rendered.
Find out how to obtain prior authorization for certain services from iowa total care, a medicaid managed care organization. Services must be a covered health plan benefit and medically necessary with prior. Member must be eligible at the time services are rendered. Services must be a covered health plan benefit and medically necessary with prior authorization as per plan policy and procedures.